By
Noel Lee J. Miranda, DVM, MSc, FPCVPH, DPCLAM
Global Health Security, One Health, and Public Health Emergency Management, Philippines
Mary Elizabeth G. Miranda, DVM, FPCVPH
CEO, Field Epidemiology Training Program Alumni Foundation, Inc, Philippines
ABSTRACT
Excessive human-animal interactions are driven by ecosystem degradation. Sustainable and safe wildlife and biodiversity management have become priority global concerns, where the One Health approach is the ultimate solution. The International Health Regulations (IHR), national action planning for health security (NAPHS), and Global Health Security (GHS) Agenda serve as the basis for the development of health security core capacities and national action plans. The IHR-Joint External Evaluation (JEE) currently covers general One Health competencies that are core to emerging infectious disease (EID) downstream prevention and mitigation. What is not explicitly mainstreamed in the JEE, NAPHS, and countries’ GHS strengthening is the upstream prevention of zoonoses spillover at source and corresponding One Health actions. Global organizations, including the World Bank and UN Quadripartite, encourage and support initiatives on zoonotic spillover prevention. This is an opportune time to strengthen GHS capabilities and integrate One Health EID prevention at source in NAPHS. The health sector’s championing of this cause is believed to be most appropriate to achieve the GHS goal. This policy paper attempts to fill the advocacy gap for the proposed mainstreaming of EID risk reduction at source in IHR-related frameworks, tools, and initiatives.
Emergence of Zoonoses in the Animal-Human-Environment Interface and One Health
The emergence of pathogens with spillover and pandemic potential (influenza, SARS, Ebola, Henipavirus) has been an ever-present threat to global health security. Zoonotic spillover and transmission risks exist within animal-human-ecosystem/environment (A-H-E) interfaces. Excessive human-animal interactions are driven by ecosystem disturbances and degradation, which are driven by various factors, such as wildlife habitat encroachment and wildlife trade. Because of the interconnectedness of biodiversity loss and human security, achieving sustainable and safe wildlife and biodiversity management have become priority global concerns, where the ultimate solution is a well-coordinated One Health response.
One Health recognizes the interconnectedness of the health and well-being of humans, animals, and the ecosystem. Achieving optimal health involves cross-sectoral collaborations in addressing health risks at the animal-human-ecosystem interface, especially ecosystem disruptions driven by human activities.
The One Health High Level Expert Panel (OHHLEP) defines One Health as an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystems. The approach mobilizes multiple sectors, disciplines, and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems while addressing the collective need for healthy food, water, energy, and air, taking action on climate change, and contributing to sustainable development.[1]
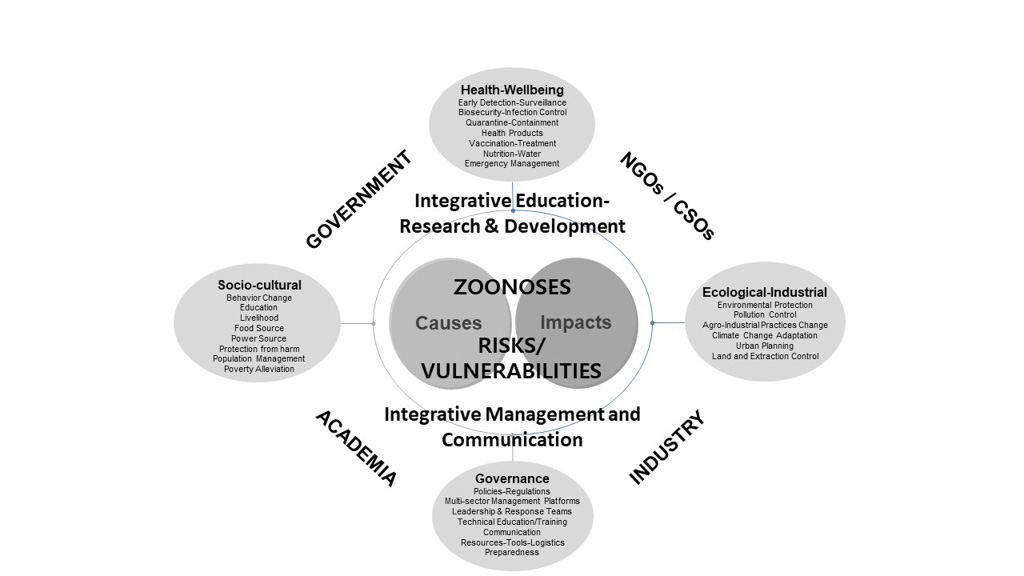
The Tripartite Guide to Addressing Zoonotic Diseases identified the relevant One Health stakeholders.[2] The envisioned interdependent multisectoral One Health system, as previously proposed, is presented in figure 1.
Figure 1. Multisectoral One Health System[3]
A keen understanding of the threats and potential long-term solutions compel countries to vigorously promote One Health approaches and to urgently mainstream strategies for ecosystem protection, restoration, and sustainable management in national action plans for health security (NAPHS)[4].
In its updated report in 2022, the World Bank highlights that prevention guided by One Health principles is estimated to cost between approximately US$10.3 billion and US$11.5 billion per year.[5] The World Bank claims that prevention costs are less than one percent of the cost of responding to the COVID-19 pandemic in one single year, 2020.
One Health within the IHR 2005, NAPHS, and the GHSA
The International Health Regulations (IHR 2005)[6], the NAPHS, and the Global Health Security Agenda (GHSA)[7] serve as the basis for the development of health security core capacities and national action plans. These are interrelated formal agreements and frameworks aiming to minimize the global impact of an outbreak. Various assessment and monitoring tools have been developed by WHO, such as the IHR Monitoring and Evaluation Framework (MEF)[8], which includes the State Party Self-Evaluation and Annual Reporting (SPAR) Tool[9], and the Joint External Evaluation (JEE) Tool- 3rd edition[10]. The prevailing expectation is for countries to target strengthening several technical areas to a level of “demonstrated capacity.” The GHSA 2024 Framework/initiative supports countries to target strengthening at least five technical areas to a level of “Demonstrated Capacity.”[11]
In relation to the current IHR-driven context, it appears that efforts to establish the One Health approach are focused on joint detection and assessment of a potentially zoonotic outbreak that emerges in a specific animal-human-environment interface and the joint response to mitigate the spread of the disease, especially sustained human to human spread and potential disease spillback from humans to animals.[12] Furthermore, One Health is promoted to enable joint decision-making on reporting the verified disease incident to WHO within 24 hours (through the national IHR Focal Point).
The JEE currently covers general One Health competencies that are core to EID prevention and mitigation. What is not explicitly mainstreamed in the JEE, NAPHS, and countries’ GHS strengthening is the prevention of zoonoses emergence/spillover at source and corresponding One Health actions, even though outbreak risk-reduction at source is a main driver of promoting One Health, and is the reason One Health has gained extraordinary attention during (not before) the COVID-19 pandemic. Therefore, the IHR-related instruments and tools merely promote secondary (downstream) prevention to mitigate the impacts of spillover events. This will likely be the prevailing situation over the next several years, as most countries are still catching up with enhancing their basic zoonotic disease detection and response core competencies. Indeed, this is a global challenge that governments need to prioritize, subject to the adoption of the policy that EID prevention at source should be mainstreamed in IHR-related initiatives.
It seems the above definition of One Health is very clear in compelling the use of the IHR JEE and SPAR tools to include a focus on the prevention of zoonotic spillover at source and inclusion of such in NAPHS. If this is not the immediate interpretation of relevant stakeholders, then emphasis must be made on how the definition is conveyed so that the message of zoonotic disease prevention at source becomes clearer.
In the Western Pacific and Southeast Asian region, the two regional offices of WHO formulated the Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies (APSED) III.[13] In it are statements drawing multisectoral collaborations towards addressing health risks at the human-animal interface through the concept of One Health. It states, “The One Health approach is primarily preventive and emphasizes the need for effective collaborative efforts…. to control emerging diseases of animal origin, contribute towards pandemic preparedness, and reduce the risk of zoonotic potential including foodborne diseases at its source.” The document, however, does not go further than these implicit statements.
One Health Focus Areas for Inclusion in NAPHS
Zoonoses risk pathways in relation to biodiversity fragility amplify the drivers for disease emergence. Understanding the drivers by investigating the complex interactions at the A-H-E interface is critical in the attempt to address bio-risks. Considering the ongoing SARS-CoV-2 pandemic, this is an opportune time to strengthen GHS capabilities and integrate One Health zoonotic spillover prevention at source in NAPHS. A One Health approach is particularly relevant to enable joint field operations planning, law enforcement, nature conservation, food animal production and market oversight, zoonosis surveillance, and rapid response to at-source threats and disease outbreaks. It is recommended that the drafting of NAPHS will be cognizant of this opportunity to encompass relevant aspects of sustainable wildlife and biodiversity management through a One Health Approach.
The call for the mainstreaming of bio-risk reduction at source is made explicit in the Quadripartite One Health Joint Plan of Action- 2022-2026, Action track 2: Reducing the risks from emerging and re-emerging zoonotic epidemics and pandemics. The document states that cohesive and collaborative global efforts that tackle emerging diseases at source are imperative. Action track 2 focuses on: i) understanding the drivers of (re-)emerging zoonotic diseases and related processes and pathways, including ecosystem degradation, land use, and habitat change, environmental and climatic factors, as well as harvesting, farming and the trade of animals, wild and domestic; ii) developing risk mitigation measures, including the maintenance of resilient, healthy ecosystems, early interventions aimed at reversing or halting environmental degradation and biodiversity loss, the regulation of farming and trade in wildlife and wild animal products, and the reduction of spillover risks at key animal value-chain points and wildlife-domestic animal-human interfaces, including live animal markets (traditional markets); and iii) enhancing sustainable and targeted One Health surveillance, early warning, and response mechanisms in ecosystems, targeting animal-human-environment interfaces and key animal value chain points.
More importantly, the Quadripartite joint plan of action emphasizes that while there will be continuing focus on known (re-)emerging zoonotic diseases previously identified to have epidemic and pandemic potential, the focus is also to be devoted to “Disease X,” caused by a yet unknown zoonotic pathogen and with the potential to develop into a future epidemic/pandemic. The OHHLEP, as the technical advisory group supporting the Quadripartite, formulated a One Health Theory of Change[14] and a whitepaper on “Prevention of Zoonotic Spillover,”[15]where the long-term outcomes included improved ecosystem protection and management, including wildlife, biodiversity, energy security, rural and urban development, and enhanced resilience of communities through better disease prevention. The whitepaper focuses on preventing a pathogen from transferring from animals to humans, i.e., the prevention of zoonotic/pathogen spillover, including all its upstream drivers.
Through its report on investing in One Health to reduce the risk of EID, the World Bank states that prevention is a solid foundation for global health security and improved development outcomes at much lower societal and economic costs.[16] Disease prevention should include One Health initiatives to reduce wildlife trade. In this light, the endorsement of ASEAN of its regional strategy for preventing transmission of zoonotic diseases from wildlife trade[17] is a positive step worth replicating elsewhere.
The World Bank report, ASEAN strategy, and the Quadripartite One Health joint plan of action provide examples of prevention approaches. The COP15 (The UN Biodiversity Conference) targets a range of relevant One Health issues in a new agreement known as the post-2020 Global Biodiversity Framework.[18] It is important to mention here that many of the issues relevant to One Health disease prevention at source also fall within the targets of Planetary Health, which is also a strong global movement.[19] Managing ecosystem degradation and biodiversity loss will prevent not just future pandemics but also other important health security threats such as food insecurity, climate change, and natural disasters and their impacts.
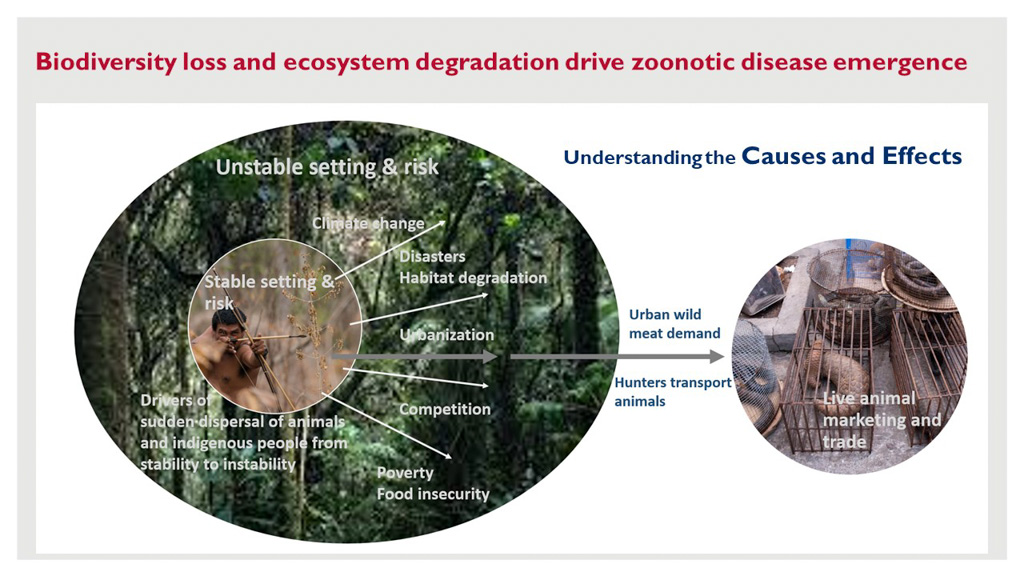
Prevention and focus on drivers of biodiversity shifts and loss should be framed around overarching themes, including poverty reduction and food and livelihood insecurity, especially involving local and indigenous communities most impacted by biodiversity shifts. The below illustrates how indigenous communities are integral to the health of the ecosystem.
Figure 2.
Generally, the key elements for inclusion in NAPHS are the various risk reduction approaches related to ecosystem and biodiversity protection, restoration, and conservation, such as on land use, expansion of agriculture, wildlife and livestock trade, production, and consumption, and pollution control, especially in critical A-H-E interfaces. The passing of enabling legislation is considered as a key action for countries to include in their agenda.
Emphasis on multisectoral One Health collaborations to address emerging pandemic threats
One Health is now globally recognized and has been promoted by the Quadripartite[20] and global institutions. However, while human health, veterinary, and environmental health sectors have collaborated to a certain extent, the desired level of One Health collaboration, also involving other relevant sectors, such as environment/biodiversity, education, and social services, has yet to be fully achieved. This situation has been recently verified by several countries’ JEEs. Many countries still lack high-level formal One Health mechanisms for multisectoral coordination and integration of activities across the human health, agricultural, and environmental/wildlife sectors. Inter-sectoral collaborations remain largely ad hoc, short-lived, and arbitrary, triggered only during disease outbreaks or when global attention is drawn towards an actual tragedy, as exemplified in the COVID-19 pandemic. Despite the large and growing body of evidence supporting the usefulness of One Health, the great majority of relevant sectors and entities continue to operate in silos.
The COVID-19 pandemic has drawn greater global commitment to strengthening One Health approaches and collaborations. This commitment is expected to enhance the development of truly multisectoral One Health collaborative structures, which are embodied in NAPHS. It should clearly describe the required One Health leadership and cohesive governance structures from local to national levels. The effective designation of the lead sector or sectors is important- One Health is founded on the principle of multisectoral collaboration and encourages joint/shared sectoral oversight and undertakings. As mentioned above, these collaborations should center on biodiversity conservation, protection, and restoration. The established system should support leadership development and enhancement— generating a cadre of professionals and civil servants with advanced competencies in One Health systems development, implementation, and management that can better enable sustained collaborations.
Discussion and Conclusion
The emergence of several novel pathogens have triggered the declarations of past PHEIC, including the COVID-19 pandemic. Many of these pathogens are present in our environment and remain undetected, and are constantly future pandemic threats, with some likely to be as or more devastating than SARS-CoV-2. This is the very reason that compels countries to urgently progress with enhancing their IHR core competencies related to One Health operationalization at the A-H-E interface where novel pandemic pathogens emerge. The complexity of spillover phenomenon within our intricate ecosystem calls for a diligent approach for modern civilization to better confront and prevent potentially catastrophic consequences. This urgent calling provides strong justification for ensuring the success of One Health as contextualized side by side with the goals of enhanced GHS at large.
Tackling the problem at its source, i.e., tackling the cause, should not be neglected while investing more in surveillance, early detection, and response, as doing so misses the bigger picture and opportunities for bio-risk reduction at the source. Predicting and detecting the spillover hazard/threat early through good surveillance is important, but it may already be too late to prevent catastrophic outcomes. Existing threats successfully detected could just signify the global failure to prevent threats in the first place.
Considering the proposal presented here, a neo-IHR perspective, as presented in the following figure, should be considered in global health security undertakings.
Figure 3.
Given the favorable thrust on prevention at source made in the Quadripartite joint plan of action and the World Bank report, the global community appears to be rallying around this cause. However, there is still a prevailing disconnect among these relevant global initiatives emerging simultaneously; for example, the Quadripartite joint plan of action does not explicitly provide supporting statements toward promoting the proposed mainstreaming within the IHR/JEE/NAPHS/GHSA core competencies. On the other hand, the World Bank report refers to the IHR 2005 and the World Organisation for Animal Health (WOAH) Codes and Manuals as being standards that are relevant to EID prevention. However, it alludes to the relevance of the WOAH Performance of Veterinary Services (PVS) pathway, rather than the IHR, in ensuring prevention competencies; it states,
“…. the IHR does not cover the capacity of veterinary services themselves, which are outside its remit. Veterinary services are, however, critically important for the prevention of diseases in animal populations; early detection of pathogenic agents, including zoonotic agents; their reporting and control; and preventing their spread. This is assessed through the PVS pathway, which provides a comprehensive evaluation of countries’ strengths and weaknesses in implementing WOAH standards. Most of the core competencies described through the PVS pathway are critical to prevention.”
This statement seems to imply that the proposed mainstreaming in the IHR is not necessary, as the WOAH PVS pathway covers prevention. It is the author’s view that WOAH’s PVS pathway merely lies in the animal health sector realm. This can easily be interpreted as encouraging siloed pathways to countries’ compliance with One Health standards. Besides, ecosystem and biodiversity management issues do not fall squarely in the animal health realm. The justifying and unifying element is global health security, which must be championed directly by the health sector, no matter where the relevant drivers of EID and potential PHEIC would fall. The global Nature for Health (N4H) trust fund, which is administered by the UN Multi-Partner Trust Fund Office, is a pivotal support mechanism that works to mainstream preventative One Health approaches and builds partnerships with policymakers, experts, and other stakeholders.[21]
Strategically, if prevention is to be mainstreamed in the NAPHS of countries, it could be specified under the heading of Zoonoses/EID. The technical areas related to ecosystem-based risk reduction at source could be detailed therein, such as sustainable wildlife and forest management, local/indigenous community outreach and livelihood development, regulations and law enforcement, land use policies, multisectoral collaboration framework, planning, and simulation exercises, etc., all being organized in the context of zoonosis prevention at the A-H-E interfaces at source; essentially aiming to reduce detrimental A-H-E interactions.
At this point, it all remains to be seen how the relevant global bodies will act on this matter in the near future. It is to be noted that the WHO established an intergovernmental negotiating body (INB) and has initiated the process of drafting a global accord on pandemics that could help deliver some of the required elements to prevent pandemic threats more effectively- expecting that this would strengthen the global governance for health security.[22] [23] The health sector’s championing of this cause is believed to be most appropriate to achieve the GHS goal. Of course, the primary intent of the IHR 2005 is emergency preparedness, detection and assessment, notification, and response, but situating this matter in the context of the IHR or the pending pandemic treaty provides the necessary high-level and formal mandate and framework to compel the achievements of specified EID prevention outputs and outcomes, as these will just be anchored to the existing obligations and accountability imposed on WHO State Parties. The same JEE and SPAR tools may be applied to measure corresponding indicators of progress. More importantly, it would logically result in countries incorporating the corresponding strategic elements in their revised or maiden NAPHS.
Considering the prevailing situation, this policy paper attempts to fill the advocacy gap for the proposed mainstreaming of EID risk reduction at source in IHR-related frameworks and initiatives. It answered the following questions: 1) Is EID risk reduction at source a key component of health security and public health emergency prevention? 2) What are the essential risk reduction core capacities, and how would it be beneficial to mainstream these in the context of the IHR and NAPHS?
[1] One Health High-Level Expert Panel (OHHLEP), Adisasmito WB, Almuhairi S, Behravesh CB, Bilivogui P, Bukachi SA, et al. (2022) One Health: A new definition for a sustainable and healthy future. PLoS Pathog 18(6): e1010537. https://doi.org/10.1371/journal.ppat.1010537
[2] Tripartite Guide to Addressing Zoonotic Diseases. http://www.fao.org/3/ca2942en/CA2942EN.pdf
[3] Miranda MEG, Miranda NLJ. Rabies Prevention in Asia: Institutionalizing Implementation Capacities. Rabies and Rabies Vaccines. 2020 May 5:103–16. doi: 10.1007/978-3-030-21084-7_6. PMCID: PMC7196719. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7196719/
[4] National Action Plan for Health Security (NAPHS). https://www.who.int/emergencies/operations/international-health-regulations-monitoring-evaluation-framework/national-action-plan-for-health-security
[5] Berthe, Franck Cesar Jean; Bali, Sulzhan Rameshwari; Batmanian, Garo J..
Putting Pandemics Behind Us: Investing in One Health to Reduce Risks of Emerging Infectious Diseases (English). Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/099530010212241754/P17840200ca7ff098091b7014001a08952e
[6] International Health Regulations. https://www.who.int/health-topics/international-health-regulations#tab=tab_1
[7] Global Health Security Agenda. https://globalhealthsecurityagenda.org/ (accessed 23 February 2023)
[8] IHR Monitoring and Evaluation Framework. https://www.who.int/emergencies/operations/international-health-regulations-monitoring-evaluation-framework
[9] State Party Self-Assessment Annual Report (SPAR). https://www.who.int/emergencies/operations/international-health-regulations-monitoring-evaluation-framework/states-parties-self-assessment-annual-reporting
[10] Joint External Evaluation (JEE). https://www.who.int/emergencies/operations/international-health-regulations-monitoring-evaluation-framework/joint-external-evaluations
[11] GHSA 2024 Framework. https://ghsa2024.files.wordpress.com/2019/11/ghsa-2024-framework.pdf
[12] JEE and NAPHS
[13] Asia Pacific strategy for emerging diseases and public health emergencies (APSED III). https://apps.who.int/iris/handle/10665/259094
[14] One Health Theory of Change. https://www.who.int/publications/m/item/one-health-theory-of-change
[15] Prevention of Zoonotic Spillover: From Relying on Response to Reducing the Risk at Source. OHHLEP whitepaper/Opinion piece. file:///F:/GHS%20Documents/ohhlep-prevention-of-zoonotic-spillover.pdf
[16] Putting Pandemics Behind Us: Investing in One Health to Reduce Risks of Emerging Infectious Diseases (English). Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/099530010212241754/P17840200ca7ff098091b7014001a08952e
[17] ASEAN regional strategy for preventing transmission of zoonotic diseases from wildlife trade – Pending publication
[18] COP15, Post-2020 Global Biodiversity Framework. https://unctad.org/topic/trade-and-environment/biotrade/Post-2020-framework
[19] Planetary Health. https://unfccc.int/climate-action/un-global-climate-action-awards/planetary-health
[20] Quadripartite One Health Joint Plan of Action. https://www.who.int/news/item/23-12-2022-one-health-joint-plan-of-action-launched-and-presented-by-who-and-the-quadripartite-partners#:~:text=The%20Quadripartite%20is%20currently%20developing,One%20Health%20systems%20and%20capacities.
[21] N4H. https://www.nature4health.net/about/ Nature for Health Biodiversity for Pandemic Prevention Multi-Partner Trust Fund; https://mptf.undp.org/fund/bhp00
[22] Putting Pandemics Behind Us: Investing in One Health to Reduce Risks of Emerging Infectious Diseases (English). Washington, D.C.: World Bank Group.
[23] Intergovernmental Negotiating Body. https://inb.who.int/
The views expressed in this article are the author’s alone, and do not necessarily reflect the official position of the DKI APCSS or the United States Government.
July 2022
Published: March 17, 2023
Category: Perspectives
Volume: 24 - 2023